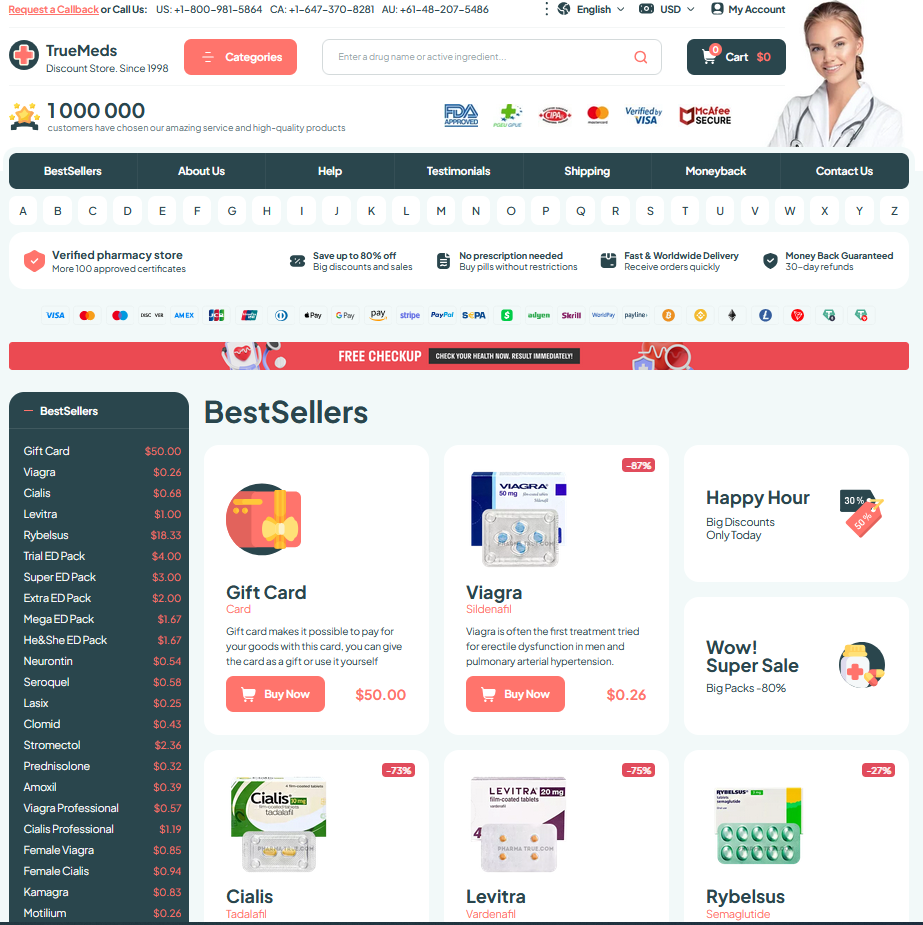
Click HERE To Buy Cymbalta Online ↓
 Tapering Off Cymbalta: Tips to Minimize Withdrawal
Tapering Off Cymbalta: Tips to Minimize Withdrawal
Plan Your Exit: Work with Your Provider
When I decided to stop Cymbalta, the first step was a conversation with my clinician about goals, timeline, and risks. I shared past side effects and daily routines so adjustments fit my life.
We mapped a slow, flexible taper, set measurable checkpoints, and agreed on signs that would trigger a pause or reassessment. My provider explained potential withdrawal symptoms and set a communication schedule for quick feedback.
| Step | Action |
|---|---|
| 1 | Plan dose changes |
Keep close contact, track symptoms daily, and don’t hesitate to consult if withdrawal intensifies; collaboration reduces surprises and improves outcomes. Documenting changes, sleep, mood, and appetite helped us fine-tune pacing without panic. This teamwork made the exit manageable. Celebrate small wins together.
Recognize Withdrawal Signals Early and Accurately

I felt a sudden fizz in my head the day after lowering my dose, an uncanny mix of vertigo and sharp electric jolts.
These sensations are common when tapering off cymbalta; mood swings, insomnia, nausea and sensory disturbances often signal early neural adaptation to change.
Track symptoms with a diary: note timing, triggers, and intensity. Patterns can reveal whether issues stem from dose reduction or other causes.
Report worrying signs promptly — severe dizziness, intense headaches, suicidal thoughts, or seizures. Timely, clear communication with clinicians ensures safer adjustments and emotional reassurance.
Slow, Individualized Tapering Beats Abrupt Stops
Leaving a medication can feel like stepping into fog, but a steady, personalized rhythm eases the path. Work with your prescriber to design a plan that reflects your history, symptom pattern, and lifestyle; even small reductions over weeks can prevent shocks to your system. When lowering cymbalta, track moods, sleep, and physical sensations daily so adjustments are informed rather than guessed, keeping withdrawal manageable and predictable. Listen to your body.
Adjustments should be patient and reversible: pause or slow reductions if symptoms spike, and consider microdosing tactics or pellet splitting under medical supervision. Supportive care—hydration, gentle exercise, stable sleep, and therapy—softens transitions and addresses emotional fallout. Keep a symptom log to share at appointments, and avoid sudden discontinuation or unapproved substitutes. With preparation, clarity, and open communication, the journey off medication becomes a collaborative, safer process that respects individual variance.
Adjust Doses Gradually Using Practical Scheduling Strategies

On a rainy morning, I halved my anxiety by breaking down the process into tiny, scheduled steps. Small percentage reductions—5–10% every two to four weeks—let your body adapt, and using pill cutters, liquid formulations, or pharmacy-compounded doses makes cymbalta reductions more precise. Keep a simple dosing calendar and set alarms so changes become routine instead of surprises.
Log symptoms daily and pair dose changes with self-care rituals like evening walks or hydration to spot patterns quickly. If withdrawal symptoms intensify, pause the decrease or return to the previous dose for stability. Communicate adjustments clearly with your clinician, and consider extending intervals between steps; slow, steady pacing often wins over rushed schedules for safer, smoother outcomes.
Manage Symptoms with Nonpharmacologic Support Techniques
When I tapered off cymbalta, small rituals anchored each day. A morning walk, a cup of tea and a short breathing practice created predictable moments that softened sudden shifts. That stability mattered more than I expected.
Track patterns: note sleep, mood, and sensations after dose changes. Journaling helps spot triggers and gauge progress without guessing.
Use nonpharmacologic supports: paced breathing, progressive muscle relaxation, gentle yoga, regular aerobic activity, and social connection. These lower intensity symptoms and reduce reliance on quick fixes.
If dizziness, insomnia, or mood swings spike, adapt routines immediately: nap, hydrate, adjust sleep hygiene, and call your provider if symptoms persist or worsen. Small changes prevent crises and preserve long-term wellbeing and resilience.
| Technique | Benefit |
|---|---|
| Breathing exercises | Reduces anxiety |
| Exercise | Boosts mood |
Know When to Seek Immediate Professional Help
A sudden, severe change—like intense suicidal thoughts, chest pain, difficulty breathing, high fever, or convulsions—should interrupt any taper. These signs require immediate medical evaluation; do not wait for your next appointment. Contact emergency services or your prescriber, and have a trusted person stay with you if possible.
Less urgent but concerning symptoms—persistent dizziness, worsening mood, hallucinations, severe insomnia, or inability to eat or drink—warrant contact with your clinician. They can adjust the taper, suggest short-term medications, or arrange assessment. Keep a medication list and symptom diary for upcoming appointments.